
The Entangler | Inside Winter 2026

Chair's Message
Welcome to the Winter 2026 edition of the Entangler
In memoriam

Remembering Professor Kostadinka Bizheva (“Dida”)
It is with great sadness that we acknowledge the passing of Kostadinka Bizheva, Professor in the Department of Physics and Astronomy, affectionately known as Dida to her colleagues and friends.
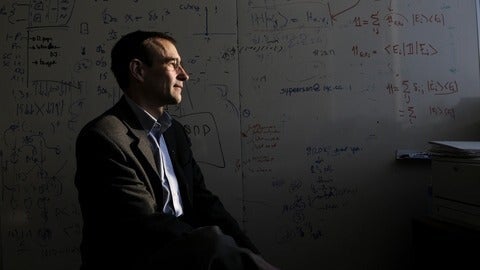
IQC and Waterloo mourn the loss of Raymond Laflamme
Raymond Laflamme, a trailblazer in quantum information processing and pioneer of IQC, died on June 19 after a lengthy battle with cancer.
Features

Quantum computers learn how to simulate quarks
Waterloo researchers have developed a new quantum computing approach that brings science closer to simulating the early universe.
Researchers at University of Waterloo’s Institute for Quantum Computing (IQC) have reached a milestone in quantum information science: using a quantum computer to simulate how matter can behave in extreme environments, like the early universe after the big bang.
Learn more in this video: The phase diagram of quantum chromodynamics in one dimension on a quantum computer

Lava planet defies expectations
Discovery of a thick atmosphere on a lava world reshapes our understanding of rocky exoplanets.
Scientists have found a planet that challenges the long-held assumption that lava planets are too hot to sustain an atmosphere. Waterloo Scientist Dr. Lisa Dang, physics and astronomy professor, and her collaborators made this discovery when they found a thick atmosphere around the rocky exoplanet TOI-561 b after flagging it as a planet of interest.
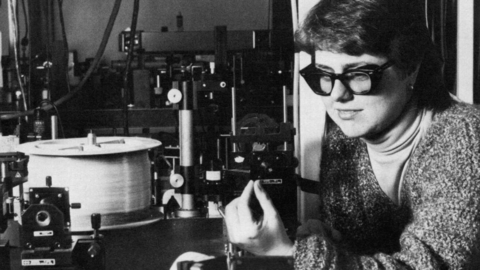
The woman behind the laser
Celebrating Dr. Donna Strickland's chirped pulse amplification breakthrough that has reshaped science, technology, and everyday life over the last 40 years.
What would you do if you woke up one day and your whole life changed?
Forty years ago, when Donna Strickland, physics professor at the University of Waterloo, and Gérard Mourou published their paper on the discovery of chirped pulse amplification (CPA), they knew they had found something that would change laser science.
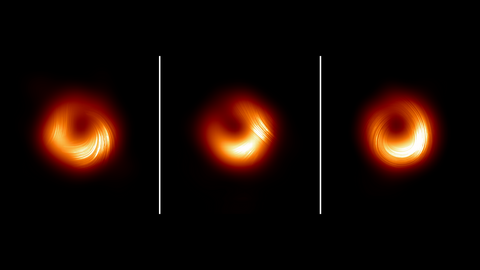
Even black holes have bad hair days
New EHT images reveal unexpected polarization flips at M87* that are giving scientists insight into the year-by-year evolution of a supermassive black hole’s ring.
The Event Horizon Telescope (EHT) collaboration has unveiled new, detailed images of M87*, the supermassive black hole at the center of the galaxy M87, that reveal a dynamic environment with changing polarization patterns near the black hole.

Will Percival named Royal Society of Canada Fellow
Dr. Will Percival, distinguished research chair in Astrophysics and director of the Waterloo Centre for Astrophysics, has been recognized as a 2025 Fellow of the Royal Society of Canada.

A fond farewell to Instructor Jeff Gardiner
The Department of Physics and Astronomy is saying goodbye to Jeff Gardiner, one of its longest serving members, who heads into retirement in October.
Meet our students

Graduating with a one-of-a-kind degree
Isabelle Marincic is the first University of Waterloo student to complete Honours Life Physics with a specialization in Biophysics and a double minor in Astrophysics and Earth Sciences.

Charting the quantum unknown
PhD student Sijia Wang explores the intersection of gravity, quantum mechanics, and information theory to illuminate the mysteries of quantum gravity.

Co-op student advances exoplanet research
Waterloo co-op student joins Caltech’s Exoplanet Technology Laboratory through a prestigious summer research program.

Mapping the universe just got easier
With new emulator, cosmologists can explore data faster than thought possible.
As the study of the universe evolves and the data sets get larger and more complex, a new breakthrough means researchers can analyze huge data sets with just a laptop and a few hours.
Clubs corner

Fall 2025: A FemPhys Review
The fall term brings along a new cohort of young physicists. For the FemPhys team, this is always an exciting time as we prepare to welcome the incoming batch of first years. We collaborated with the Faculty of Science orientation team’s Successful Scientists event to introduce the incoming class to FemPhys.

MNS Society: Fall 2025 in Review
The Fall 2025 term was a vibrant and community-driven term for the MNS Society. With a diverse lineup of events that blended science, creativity, and connection, the term brought together students from across all years and programs with something for everyone. Here’s a closer look at the events that defined our term.
SIN bin
Can you solve it? The Sir Isaac Newton Exam, as we all know and love it, continues to offer challenging problems to high school students around the world. Flex your Physics brains with this problem from a past Sir Isaac Newton Exam!

Sin Bin: 82
According to the Goodness book of Records, someone climbed the Empire State Building (1570 steps high at 24cm/step) in 12.5 minutes. According to the basic laws of physics, about how long would the trip back down take?
Sin Bin: 90
A polar bear, of mass 1250kg, sits at rest on a flat-topped chunk of ice floating as shown with its top at water level (bearly submerged??). The density of the ice is 925 kg/m3 and the density of the water is 1030 kg/m3. (After all it is salt water, silly!). Calculate the mass of the chunk of ice.