A presentation at the 2024 Eye Data and AI Summit
By Professor Helen Chen
Health Informatics
University of Waterloo
Background
- Eye and vision disorders have great implications for the individual, leading to loss of independence, which can compromise many life’s paths.
- More than 5.5 million Canadians have one of the four major eye diseases (cataracts, age-related macular degeneration, glaucoma, diabetic retinopathy) and are at serious risk of losing their vision.After age 40, the number of cases of vision loss doubles every decade. At age 75, it triples. By age 65, 1 in 9 Canadians develop irreversible vision loss and by age 75, this increases to 1 in 4. (1)
- More specifically, in Canada , there are over 2 million currently living with a seeing disability, and due to ageing and other factors, that number is in the process of doubling over the next 25 years, leading to national health care costs of over $30 billion per year (2)
- Canadians rank maintaining vision health and preventing vision loss among their top 3 health priorities.

Frequency of Eye Examination
|
Age |
Eye Examination Frequency |
|---|---|
|
Birth to 24 months |
Undergo the first eye examination |
|
2 to 5 years |
Undergo one eye examination between the ages |
|
6 to 19 years |
Undergo an eye examination annually |
|
20 to 39 years |
Undergo an eye examination every 2 to 3 years |
|
40 to 64 years |
Undergo an eye examination every 2 years |
|
65 years or older |
Undergo an eye examination annually |
Data in Eye Care

- Diagnose
- Treatment
- Manage and Prevent
- Diseases and disorders of the eye, visual system, and its related structures.
Capacity Gaps: Geographic Factors
Canada’s rural population increased by 26,609 people (+0.4%) from 2016 to reach 6.6 million in 2021.
- Increasing aging population
- “First Nations people may be at higher risk for not receiving screening eye examinations for several reasons, such as remoteness from care providers and comorbidity, as well as financial and cultural barriers” (Campbell, et al. 2020)
Optometrists practicing in rural and remote settings may face several specific challenges
- Lack of primary care providers
- Possible emergency department/clinic closures
- Acute shortages in health care workers and recruitment.
- Travel time for rural residents to access healthcare services such as eye care is significant.
Data Gaps: Eye Data Collection
Data repositories and registries are powerful tools for analyzing and presenting early diagnosis and screening programs, treatment response, health care planning, decision-making, and disease control programs
- CIHI, CCO, ORN, Ministry of Health (400+ datasets)
Eye data repository through the American Academy of Ophthalmology’s IRIS Registry (Intelligent Research in Sight).
- Includes comprehensive data on eye conditions, treatments, and outcomes collected from participating ophthalmologists nationwide (AAO, IRIS Registry).
Canada lacks a comprehensive eye data repository.
- The fragmented nature of current eye health data collection leads to inefficiencies and challenges in providing comprehensive care and innovation.
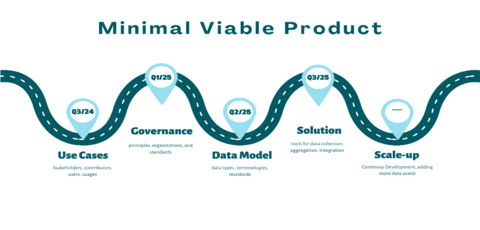
CAN-VIEW VISION
As a national data repository for Vision Care, CAN-VIEW aims to enable evidence-based policy-making and AI-powered innovations to enhance vision care and disease prevention for all Canadians.
Use Case I: Data on Population Eye Health and Service Quality
Provide data on access (service) and quality on multiple granularity
- Clinics
- Regional
- Provincial: resource allocation, budget, etc
- National: population eye health, equitable service
Use Case IIa: Reducing Documentation and Reporting Burden
- Harmonization of terminology and reporting standards
- Automation of data reporting and auditing trail for compliance

Use Case IIb: AI-Powered Data Standardization
Data may not be standardized in different electronic eye care systems
Example: Translating Rx from EMR systems to standardized RxNorm is challenging:
- Display values may not match RxNorm concept, dosing, strength, Dose Forms and Dose Form Groups
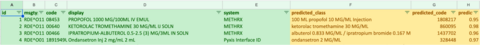
Key Observations (Non-standard EMRs)
Display data usually has all the necessary information as RxNorm but just messier:
- PROPOFOL (Name) 1000 MG/100ML (Strength) IV EMUL (Form)
Translation to RxNorm need to identify and translate key elements of messy data for Name, Strength, and Dose Form with either logic or AI
Non-standard EHRs contain all important information, while only lacking a mapping to data standards.
Where could AI Help in Data Standardization and Harmonization?
- Exact String Matching
- Partial String Match - missing values
- Embedding Models - simple AI model
- Embedding models map all concepts of RxNorm on values of Name, Strength, and Dose Form
- Translated EMR Rx can be mapped into that same format of Name, Strength, and Dose Form
- The closest RxNorm concept to the EMR Rx in the same space is the top candidate
Use Case III: Research and Innovation
- Clinical trial
- Real-world evidence
- Technology and AI innovation

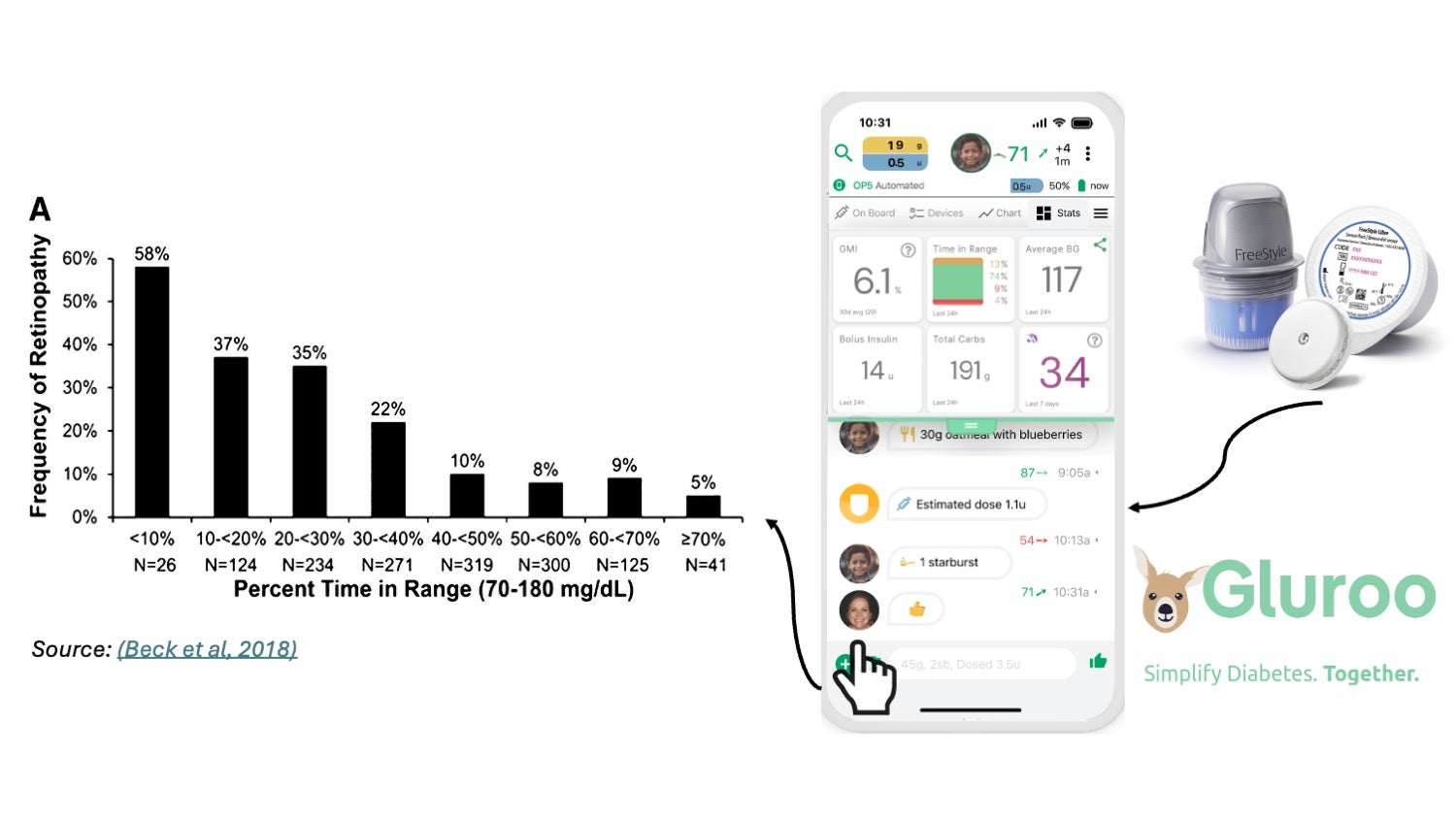
Demo: Integrating Diabetic Retinopathy Data with Glucomonitoring and Eye Morphologist Data
Problem Statement
Diabetic patients are at high risk for retinopathy, a condition that can lead to blindness if not properly monitored and managed. While glucomonitors track blood glucose levels and eye morphologists analyze retinal images, these data sources often remain siloed, limiting comprehensive patient care.
Solution
Integrate periodic data from glucomonitors and eye morphologists into the centralized eye data repository. This integration enables comprehensive monitoring and management of diabetic retinopathy while avoiding the need for continuous data streaming.
Data Collection
Readings from Glucomonitors and images from Eye Morphologists
Data Integration
Securely transfer data from glucomonitors and eye morphologists to the eye data repository
Data Analysis
Use AI and machine learning algorithms to analyze integrated data, identifying patterns and correlations between blood glucose levels and retinal changes. Provide predictive insights and early warnings for potential retinopathy developments
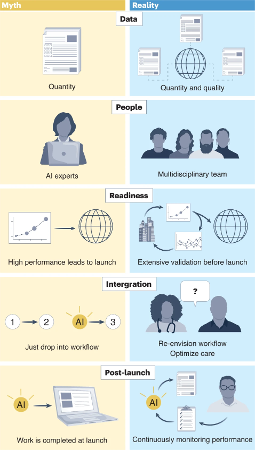
Lessons Learned from Deploying AI into Healthcare (ARDA)
|
Myth |
Reality |
|---|---|
|
More data means better AI models |
Although adequate data volume is important for developing an accurate AI model, data and label quality matters more, especially as the quantity becomes less critical as AI advances. |
|
Only AI experts are needed |
Although AI experts are core contributors in developing medical AI models, building a complete, well-functioning AI system takes a village of multidisciplinary team members. |
|
AI performance leads to clinical confidence |
Building users’ confidence in using medical AI takes time and careful validations. |
|
Integrating AI into routine workflows is straightforward |
AI should be designed around humans, not the other way around. |
|
Launch means success |
Ensure AI’s high-quality performance through continuous monitoring and iterations. |
Continuous Glucose Monitoring Systems and Eye Care
Continuous glucose monitoring systems provide real-time data on blood sugar levels, which can help predict and manage diabetic retinopathy more effectively.
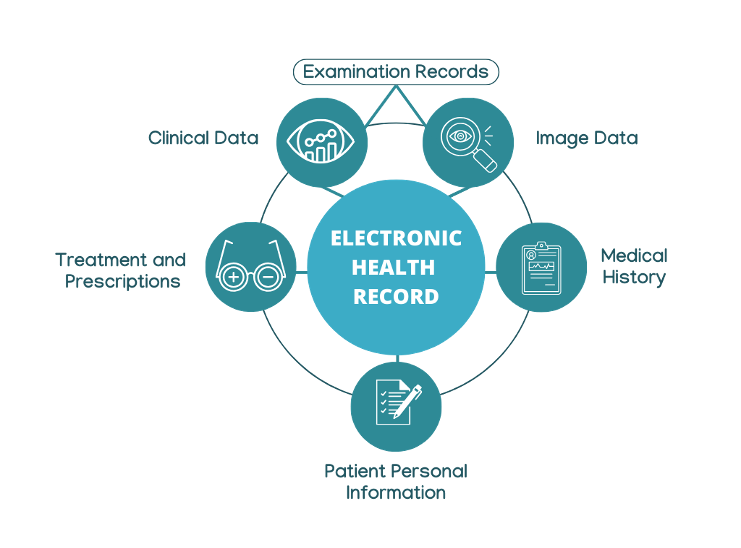
Optometry Data Model
The Optometry Data Model outlines the essential components to support comprehensive and patient-centered eye care.
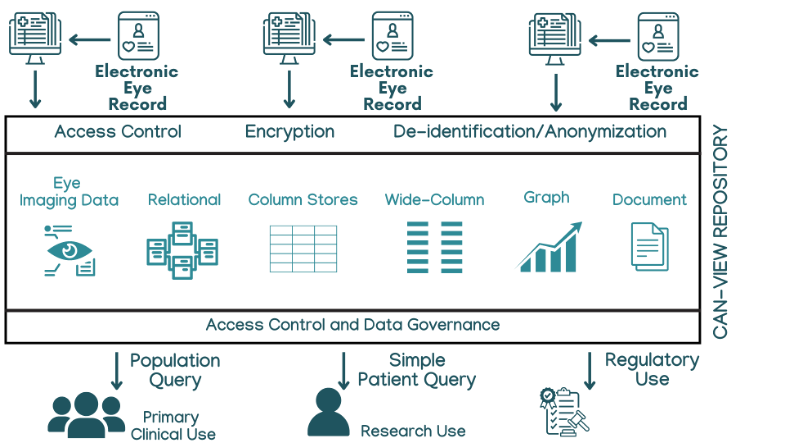
CAN-VIEW Repository Architecture
The CAN-VIEW Repository Architecture is designed to securely manage and share eye health data across Canada, enabling AI-driven insights and policy innovation. It ensures that information is protected while allowing authorized stakeholders—clinicians, researchers, and policymakers—to access the data they need for improving vision care outcomes.
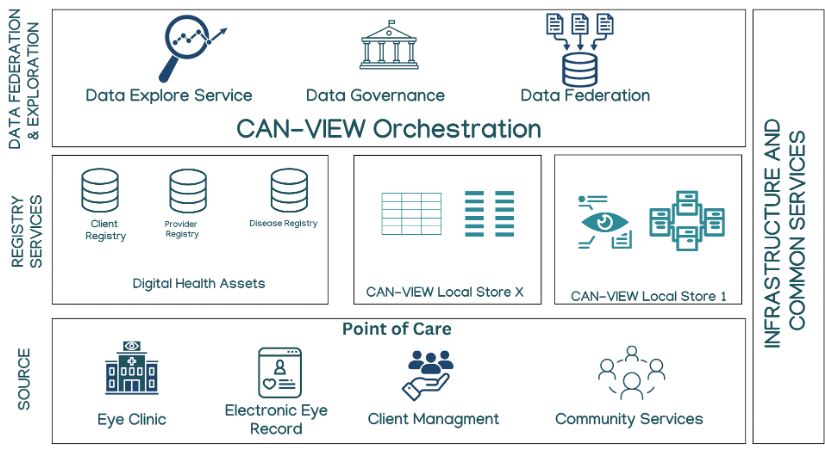
National CAN-VIEW Architecture: Federation
The National CAN-VIEW Architecture allows individual provinces, clinics, and institutions to maintain control over their data while contributing to a unified national repository—ensuring privacy, interoperability, and equitable access to eye health insights for research, policy, and innovation.
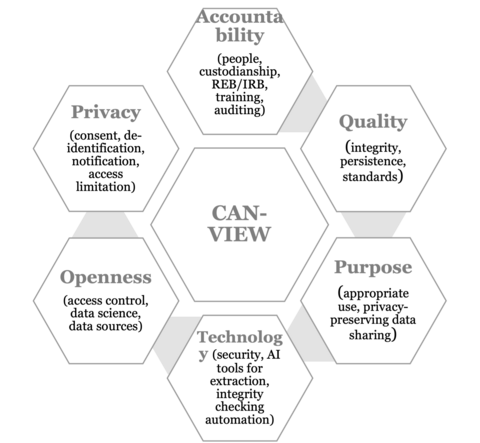
CAN-VIEW Data Governance
The CAN-VIEW Data Governance framework ensures that the national eye data repository operates with integrity, transparency, and privacy at its core.
It is built on six pillars: Accountability (clear custodianship and oversight), Quality (data standards and persistence), Purpose (appropriate and ethical use), Technology (secure infrastructure and AI tools), Openness (controlled access and collaboration), and Privacy (consent, de-identification, and access limitations)—all working together to support trustworthy data sharing and innovation in vision care.
How can we get there?
Use Case Template
|
Components |
Description |
|---|---|
|
Use Case Overview |
A summary of the situation or problem |
|
Actors (ex. optometrists, patients, researchers) |
Users who participate in use case actions |
|
Pre-condition |
Pre-case requirements that must be met before the use case can be executed |
|
Post-conditions |
Expected outcome or change that will occur after the use case is executed |
|
Main Flow |
It is the sequence of actions taken by the actors to achieve their objectives. |
|
Alternative flow |
Alternative path or variation that might occur within the use case. What was the trigger? |
Together, through CAN-VIEW, we can build a future where every Canadian has access to equitable, data-driven vision care—powered by collaboration, innovation, and trust.