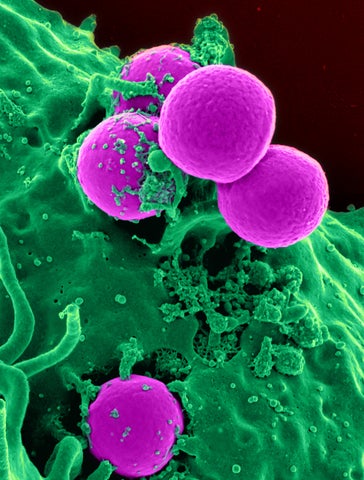
Scanning electron micrograph of a human neutrophil ingesting MRSA (Source: National Institutes of Health (NIH))
MRSA (Methicillin-resistant Staphylococcus aureus) is an antibiotic-resistant bacterial infection. Every year, around 20,000 new MRSA cases are observed in Canada, mostly in hospitals. Due to its antibiotic resistance, MRSA is a very difficult and expensive disease to treat. An MRSA outbreak in a hospital may render a significant portion of the hospital’s room and lab capacity useless during quarantine and sanitization processes. Roommates of nosocomial methicillin-resistant Staphylococcus aureus (MRSA) cases have a high risk of MRSA acquisition, e.g., around 8%. Therefore, infection prevention and control guidelines recommend that these individuals be isolated and undergo surveillance testing, and around 80% of Ontario Canadian hospitals employ some form of MRSA surveillance practices for the exposed roommates. However, practices vary and the optimal surveillance testing and isolation strategies are unknown.
We develop a stochastic dynamic programming model to optimize testing and isolation decisions for the contacts of index MRSA cases in hospitals to minimize the loss of quality-adjusted life years and the number of MRSA colonizations. Our model provides a novel framework that formulates the problem as a Markov decision process, capturing the partial observability of patients’ health states by keeping sufficient information within the model state and dynamically incorporating new test results, thereby overcoming the curse of dimensionality associated with partially observable Markov decision processes. We optimally solve the model using clinical data from a Canadian community hospital and conduct sensitivity analyses on key parameters, including disutility values and disease parameters.
We computationally analyze the structure of the optimal testing decisions, which recommend varying the frequency and timing of tests based on initial test results and room configurations. In some cases, optimal testing protocols may delay testing to improve test sensitivities due to the increasing bacterial load. However, in case of aggressive disease transmission, earlier testing may become optimal to detect colonized roommates early and prevent transmissions in isolation. Optimal testing decisions offer valuable insight for policymakers in improving health outcomes while reducing associated costs compared to current guidelines and practices. Optimal testing decisions reduce the loss of quality-adjusted life years by 18.9%, MRSA colonizations by 3.4%, and total costs by 36. 3% compared to the guidelines in the base case. In addition, we compare the performances of various practical MRSA testing protocols using the proposed modeling framework and determine those with close-to-optimal performance while balancing clinical efficacy and cost-effectiveness. The proposed modeling framework can be applied to other healthcare-associated infections and infectious diseases.