We know that we should apply the hierarchy of controls when thinking about musculoskeletal disorders
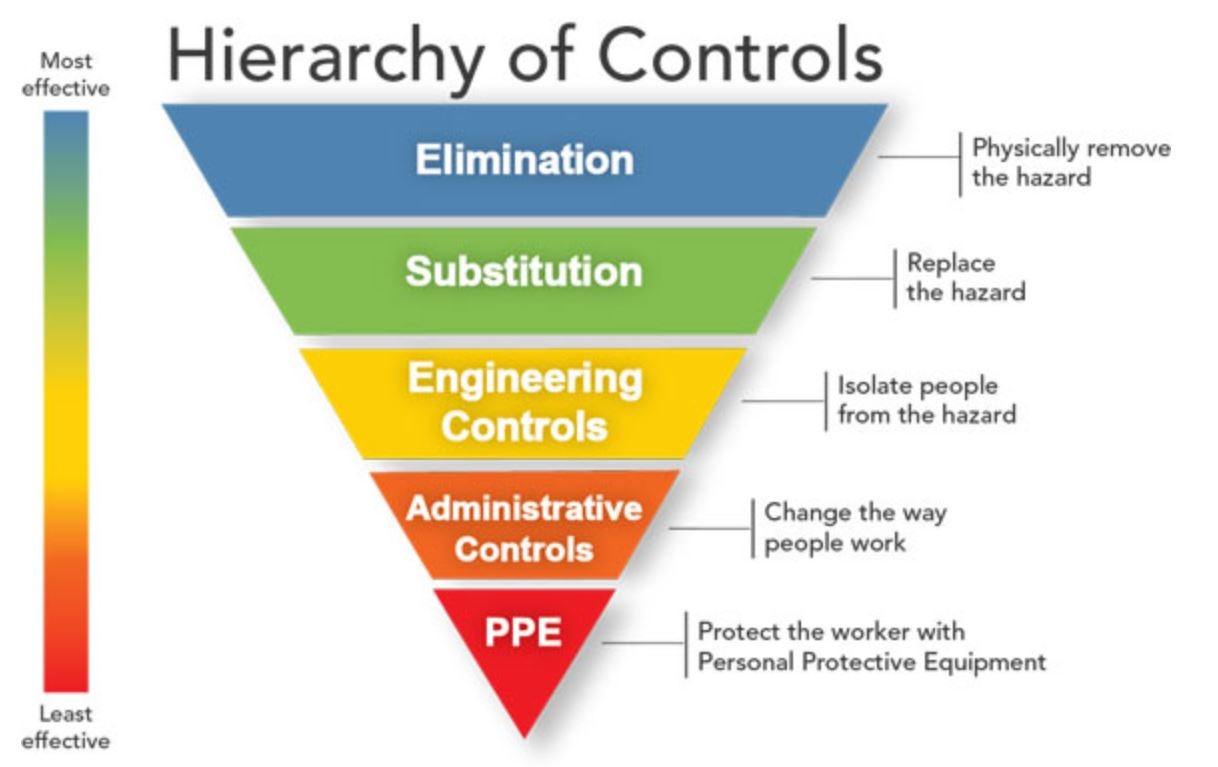
(MSDs), but in some work situations we can’t design out risk (at least not in the foreseeable future). Take paramedics for example. While evidence shows that some MSD risks can be designed out, for example by adding powered stretcher and load systems (Armstrong et al., 2017), forceful exertions are still necessary to provide timely patient care and MSDs still remain high. The same situation may be true for other healthcare workers like nurses, or healthcare aids who may simply have to exert physical forces to provide timely patient care during job tasks that are difficult to modify through other means (at least in the short term). So, what can we do to reduce MSD risks for those work tasks that may not be so easily modified? Maybe we need to think a little more about how we can better fit the worker to the work.
So, what does it mean to fit the worker to the work? Well, if we boil it down, we want to ensure that a worker has both the physical capacity and movement competency necessary to meet the demands of their non-modifiable work tasks. To illustrate this concept, we use the Demand-Capacity-Competency model. By modelling the interaction between the demands of work and the capacity of workers using a teeter totter like scale, we suggest that strategies to increase a worker’s underlying capacity (for example, by providing targeted strength and conditioning) could increase their ability to safely meet the demands of their (non-modifiable) work. However, using the Demand-Capacity-Competency diagram, we can also view the fulcrum as movement competency, or how an individual moves to leverage their capacity. This means that interventions targeted to improving movement competency should also increase a worker’s ability to more effectively apply their capacity in order to meet (non-modifiable) job demands.
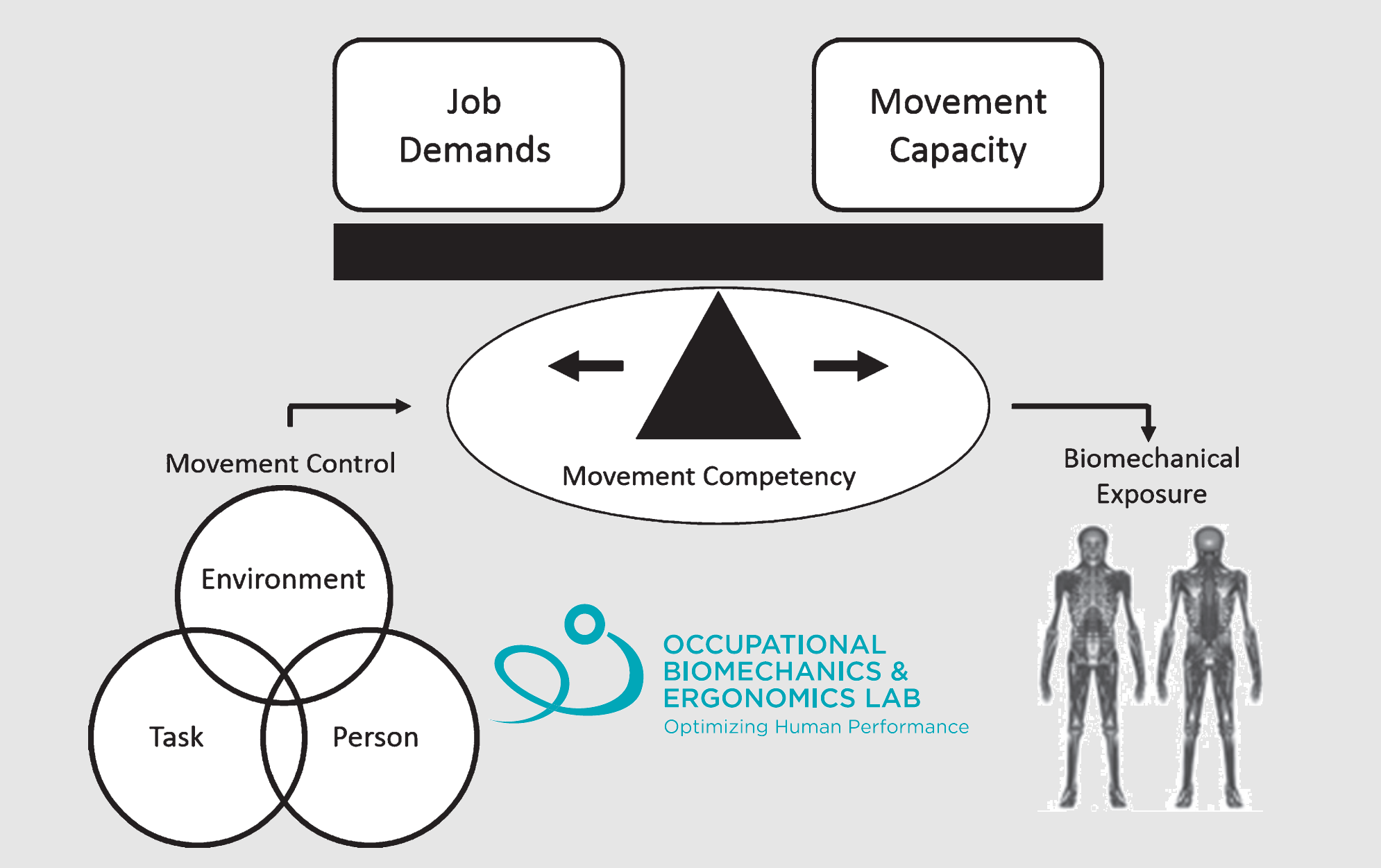
Figure 1: A visualization of our Demands-Capacity-Competency model. We have used this model to understand how we can ‘tip the scales to the right for musculoskeletal disorder prevention’ by reducing demands, increasing capacity, or leveraging movement competency. Figure adapted from Armstrong et al. (2019).
Recently, we applied this model to inform our thinking about developing a strength and conditioning program to enhance paramedics physical readiness for duty. In a paper recently published in Work, we learned that structured strength and conditioning (this study used a 4-week 3 session / week program) increased paramedics performance on a physical employment standard (a test to measure ones ability to meet the physical demands of paramedic work). Diving deeper, first we identified that the ability to generate power through the lower body was a significant predictor of one’s ability to time-efficiently perform a series of demanding paramedic tasks like carrying a backboard and loading a stretcher into an ambulance. Second, we targeted a portion of the strength and condition towards improving lower body power (though in some cases, we need to help trainees build up to the point where they could focus on power). Though this only provides one example, growing evidence supports the hypothesis that increasing one’s physical capacity (for example through resistance training), can help prevent and manage MSDs (see van Eerd et al., 2016 for a nice review focussed on the prevention of upper extremity MSDs). For work with non-modifiable, or difficult to modify tasks, developing programs to help workers improve their physical capacities may provide a great opportunity to prevent MSD.
Let’s change gears and talk about movement competency. Both within our lab’s previous work (i.e., Armstrong et al., 2021), and in the literature more broadly (i.e., Kingma et al., 2004), there is evidence demonstrating that the way an individual moves when completing physically demanding work tasks can influence the resultant biomechanical exposures on their body. This evidence may explain why education and training on lifting mechanics (as one example) has become common place in many work settings. But this brings up an interesting point; training on safe handling technique doesn’t work!? Well, at least not when we assume that if we tell people to move differently, they will simply listen and move differently…
We have spent a lot of time trying to reconcile our hypothesis that improved movement competency (i.e., the ability to safely leverage one’s capacity) should reduce MSD with the IRRST review paper indicating that safe handling technique training is questionable as an MSD prevention strategy. To move this conversation forward, we argue that we need to dig a little deeper to understand why workers move the way they do. At this point, most people have likely heard the saying “lift with your legs, not your back”, so maybe knowledge of what to do isn’t the missing piece? Understanding why people move they way they do is an important pre-cursor to helping people move in different ways. To help guide our thinking and continued research we incorporate motor control based theoretical paradigms to help us understand why people move the way they do, or posed differently, what a mover tries to optimize when selecting a movement strategy.
Leveraging the grand unified theory of sports performance posed by Glazier, attempting to change a workers movement competency (or movement behaviour) may require a little more effort than a chalk talk on technique (Figure 2). Within this framework the interaction of personal, environmental and task factors likely influence how a worker thinks about moving to complete their work tasks. Viewed from a motor control perspective, we might consider this as the motor control objective function (i.e., best way to move in order to complete the task goal, subject to constraints). Therefore, it may be of critical importance to first understand the movement objectives that a worker has decided on and maybe also personal level constraints (i.e., insufficient ankle range of motion to squat down) before attempting to improve their movement competency.
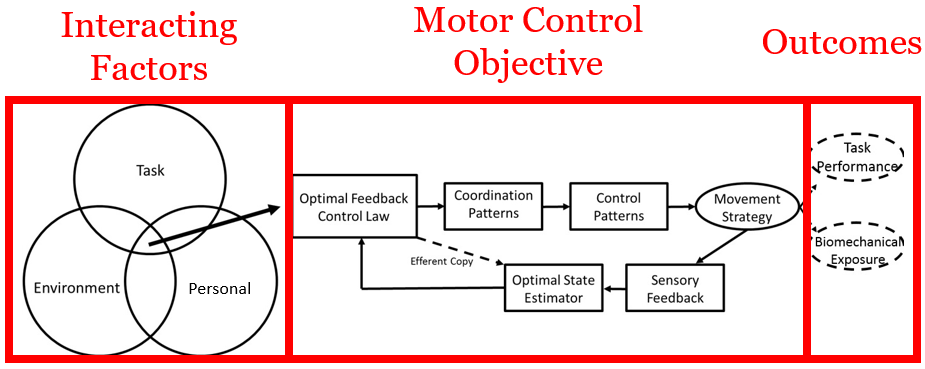
Figure 2: Theoretical framework used to understand determinants of a worker’s movement strategy. Based on this framework interacting personal, environment and task factors will influence the definition of a worker’s motor control objectives. The defined motor control objectives will influence a worker’s movement strategy, which will have associated task performance and biomechanical exposure outcomes of interest. Figure adopted from Armstrong & Fischer (2020).
It is still early days for us as we continue to explore ways to uncover individual level control strategies, but our preliminary research in this area shows promise. Considering a backboard lifting task, we hypothesized that some workers would lift in a way that minimized the biomechanical exposures at the low back and others would not. In other words, we believed that some lifters might actually perceive the torque about their spine and aim to move in ways which kept those torques as consistently low as possible (i.e., low magnitude and low trial-to-trial variability). Our hypothesis was supported, where we found that lifters with lower magnitudes of low back biomechanical exposures also had less variability in these exposures. Though we did not directly test each lifter’s ability to perceive torque at the spine, we think this might mean that to train movement competency, we might first want to ensure that workers can effectively perceive and make used of perceptive information about how their body feels when lifting. This might enable those lifters to better consider biomechanical exposure when they choose their lifting strategies. Could you image a lift training session focussed on improving proprioception and kinesthetic sense as a means to reduce MSDs? We’re not sure if it would work either, but early findings support that it might not be a bad idea if we truly want to improve movement competency as an MSD prevention strategy.
Developing effective worker-focused ergonomic interventions to reduce MSD risk for sectors with non-modifiable job demands is an ongoing need and is not a problem that is easy to address. However, we believe that understanding why workers move the way they do by considering movement strategy through a motor control lens shows promise for the potential to develop effective worker-focused ergonomic interventions. We hope that in the future such interventions will have MSD prevention benefits to work sectors with non-modifiable demands, such as paramedicine. Stay tuned as we hope to have exciting updates on this research direction to share with you in the future!
For more information on worker-focused interventions developed for the paramedic please check out our CRE-MSD webinar:
If you are interested in discussing ways to fit the worker to work further please feel free to connect on twitter (@dparmstr or @BiomechErgoLab), LinkedIn (https://www.linkedin.com/in/daniel-armstrong-90239b1b7/) or by email (dparmstr@uwaterloo.ca).