Dr. Sarah MacIver on dry eye disease
What is dry eye?
Dry eye disease, or simply dry eye, is a chronic condition that occurs when an individual does not produce enough quality tears to properly lubricate their eyes. It is estimated that up to 30% of Canadians suffer from dry eye. In the coming years, this number is expected to increase as the population ages.
Tears are made up of a variety of substances that each contribute to the overall function of the eye. Each time you blink, your eyelids spread tears over the surface of the eye, creating a tear film.
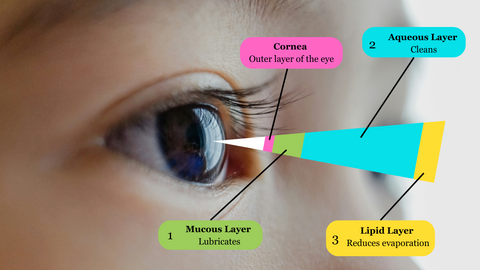
The composition of the tear film can be broken up into three main layers:
-
The inner mucus layer helps the tear adhere to the surface of the eye and provides lubrication.
-
The watery middle layer keeps the eye hydrated and washes away bacteria and debris.
-
The oily outer layer prevents evaporation of the inner two layers and creates a smooth surface to see through.
When a layer is disrupted, the tear film's quality diminishes, leaving the eye vulnerable to conditions like dry eye disease.
Dry eye can be quite debilitating, since it can be painful and affect a person’s vision. Everyday tasks like using the computer or holding a conversation can become difficult.
Causes
A disrupted tear film has two main causes: insufficient tear production or too much evaporation. Either of these factors can be the sole cause of dry eye or they can work together.
Inadequate tear production can be a result of:
-
Age (tear production naturally decreases with age)
-
Preservatives in eye drops (chronic use can impact production and maintenance of the tear film)
-
Refractive eye surgery like LASIK (can reduce sensitivity to moisture needs, so the eye may not know when to produce more tears)
-
Some medications
-
Medical conditions (rheumatoid arthritis, lupus, Grave’s disease, Sjrogren’s syndrome, etc.)
Too much evaporation of the tear film can occur because of:
-
Dry, windy or smoky environments
-
Reduced blink rate (such as during prolonged computer use)
-
Contact lenses (lenses absorb tears)
-
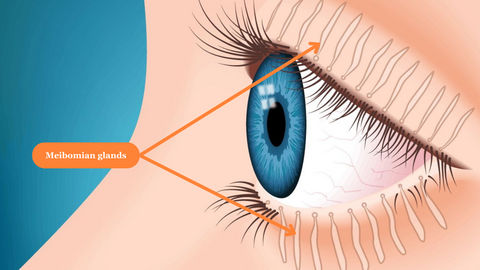
Meibomian gland dysfunction (decreases the quality/amount of oil produced)
Symptoms
Dry eye is typically a progressive disease, meaning it increases in severity over time. Mild dry eye can be characterized by some burning, stinging or itching due to the lack of proper lubrication on the surface of the eye. Grittiness, a feeling of dryness and redness may also be present. A smooth and healthy tear film is needed to see clearly, so blurry vision can also occur. As a result, patients might notice themselves blinking more or rubbing their eyes to try and focus their vision.
While it may seem counterintuitive, watery eyes are also something to look out for. If the meibomian glands are not producing enough oil to keep evaporation at bay, the aqueous-producing lacrimal glands will go into overdrive to compensate.
As dry eye progresses, stinging, grittiness, redness and wateriness worsen. Light sensitivity may become prevalent, because as the surface of the eye becomes drier, light becomes scattered as it enters the eye.
The consequences from untreated severe dry eye can be serious. With minimal lubrication and moisture, the cornea (surface of the iris and pupil) is vulnerable to scratches from dust, hair or other foreign bodies that become trapped between the eye and the eyelid. Abrasions can also occur if the eyelid becomes stuck on the cornea, such as when waking from sleep. Corneal abrasions are extremely painful and can lead to infections.
Minor corneal abrasions typically heal within a few days – however, dry eye can slow healing. Deep scratches or poorly healed abrasions can cause corneal scarring, which can be permanent. Scarring prevents light from entering the eye correctly, which can cause blurry or decreased vision.
Diagnosis
Diagnosis usually starts with a comprehensive eye exam. If your optometrist suspects you have dry eye, specific tests can be performed to measure the volume and composition of tears produced to determine if you suffer from dry eye disease.
Preliminary tests may include:
-
Slit lamp test: Used to determine if your eyes produce enough tears. First, your optometrist will dilate your eyes with drops, then look into them with a microscope and thin bright light. This test is not painful, but your eyes may momentarily sting from the dilating drops and be sensitive to light afterwards.
-
Schirmir test: Also used to determine adequate tear production. Numbing drops will be put into your eyes and then a strip of paper will be placed between each eye and lower lid. You’ll be asked to gently close your eyes for five minutes. Afterwards, your optometrist will measure how much of the paper became moist. This test is generally not painful but may be slightly irritating while the paper is on the eye.
-
Tear break up time test: Used to determine how fast tears evaporate from the surface of the eye. Your optometrist will place a drop of dye into your eye and ask you to blink until the entire eye is covered. Then, you’ll look forward without blinking, while the optometrist monitors how long it takes for patches to appear in the dye. Patchy spots indicate places where parts of the tear film have evaporated. Until you blink at the end of the test, you may feel some discomfort as the surface of the eye gets drier.
To determine the exact cause of your dry eye, your optometrist will also assess the overall health of the eye, evaluate your vision, and use the results of any relevant tests to come to a final diagnosis.
Treatment
Environmental or lifestyle changes are often among the first steps in dry eye treatment. Investing in a humidifier, taking frequent breaks during screen time, or wearing sunglasses to shield your eyes from wind may help combat dry eye symptoms. Warm compresses at night can help facilitate tear production and unclog meibomian glands.
Artificial tears are also a common first line of defense. These can be purchased without a prescription and help to lubricate and retain moisture on the surface of the eyes.
If a patient still suffers from dry eye symptoms, further measures can be taken. Some prescription medications can be used to treat dry eye by stimulating the production of tears or reducing inflammation of the eyelid to prevent clogging of the meibomian glands.
Other alternatives could include the placement of an insert that slowly dissolves into a lubricating substance between the lower lid and eyeball. Another treatment option could involve plugging your tear ducts. This is a straightforward and painless procedure that typically happens in office. Your eye doctor may numb your eyes before quickly placing plugs into your tear ducts. Temporary plugs are generally made of collagen, so they dissolve over time, while permanent plugs are usually made of silicone. Tears drain from the eyes through tear ducts, so plugging these channels can also help to keep both natural and artificial tears on the surface of the eye.
As dry eye increases in severity, special scleral lenses may be used as a treatment option. While normal contact lenses can contribute to dry eye symptoms by absorbing moisture, specialty scleral lenses do the opposite by creating a pocket of lubrication over the cornea. Scleral lenses are larger than normal contact lenses. They dome over the cornea and rest on the sclera – the white part of the eye.
Severe dry eye may be treated with platelet-rich plasma drops. They are derived from a sample of a patient’s own blood. During the production process, red blood cells, white blood cells and most of the plasma are removed. Platelets and a small amount of plasma are left behind. Further processing ultimately creates a personalized eye drop that contains the same molecules as the patient’s natural tears – just in a more potent, concentrated form.

Person using a hot-compress for their eyes
Waterloo Eye Institute patients
Dry eye disease is commonly treated at the Waterloo Eye Institute. For initial diagnosis, comprehensive eye examinations are available for patients of all ages and abilities.
As of 2025, a comprehensive eye exam costs $120, while a follow-up visit costs $75. University of Waterloo employees, students and their dependants are eligible for discounts. All fees are subject to change. Patients who are under 19 or who have certain sight-threatening conditions may have one eye exam and up to two follow-ups a year covered under OHIP. People over 65 can have one eye exam and up to two follow-ups covered every 18 months.
Based on the recommendations of your optometrist, you can purchase over-the-counter artificial tears without a prescription. Pricing will be dependent on the brand and quantity, but $15-$30 is common. Microwavable eye compresses can also be purchased at the Waterloo Eye Institute, your local drugstore or online. Generally, you can expect to pay $15-$35.
Patients with moderate to severe dry eye disease may be referred to our on-site Ocular Disease Service, which includes a Dry Eye Service, for specialized ongoing care. Full and follow-up assessments cost $120 and $75 respectively.
If you are referred to our Dry Eye Service, you may decide to pursue specialized dry eye testing, which carries extra costs. During a Dry Eye Service appointment, your optometrist will analyze the health of your eye more thoroughly, in a way specific to dry eye disease.
You can book a comprehensive eye examination online or call our Primary Eye Care Service directly at 519-888-4062 (Waterloo Clinic) or 519-888-4455 (Kitchener Clinic).
Research
The University of Waterloo School of Optometry and Vision Science is ranked fifth worldwide in research output for schools of optometry. Currently, our researchers are actively looking to better understand how the cellular aging process in the cornea, conjunctiva (contains glands that produce mucus and aqueous tears) and meibomian glands affects dry eye.
Related research is underway to understand how aging is linked to the inflammatory response in the eye. This is an important avenue to explore since inflammation causes damage to the eye tissue, which leads to more dryness and inflammation.
Interested in participating in our research? Check out our current studies recruiting participants.
Article and video by Tienna Schade
Reviewed by Dr. Sarah MacIver, BSc, OD, Ocular Disease residency, FAAO
Contact
Dry eye care is offered as part of our Ocular Disease Service, located at our Waterloo Clinic. Appointments must be made by phone. Call 519-888-4623.
Address: Unit C, 419 Phillip St., Waterloo