Controlling the time and sequence of cancer therapies may hold the key to unlocking better outcomes for patients with aggressive cancers, according to research published today.
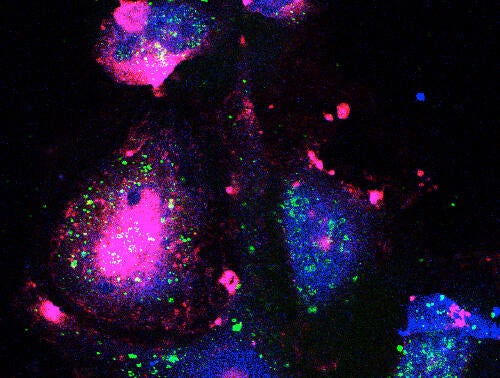 Image depicts drug-tolerant cells. Nuclear translocation of HCK drives anti-apoptotic signaling in response to taxane chemotherapy. This process is initiated by phenotypic plasticity coordinated by cell surface scaffolding involving Caveolin-1 and CD44 glycoprotein.
Image depicts drug-tolerant cells. Nuclear translocation of HCK drives anti-apoptotic signaling in response to taxane chemotherapy. This process is initiated by phenotypic plasticity coordinated by cell surface scaffolding involving Caveolin-1 and CD44 glycoprotein.
In a collaborative effort between cancer biologists at Harvard Medical School and applied mathematicians at the University of Waterloo, researchers are now showing that improved cancer therapy can be achieved by targeting drug-resistant cancer cells in a new way.
Dr. Shiladitya Sengupta and Dr. Aaron Goldman, cancer biologists at Harvard Medical School, led the research which is published in the journal Nature Communications. The team found that targeting cancer cells that survive a cancer therapy known as cytotoxic chemotherapy - with specific combinations of therapies - kills cancer cells in the lab, reduces tumors and extends the survival of mice with cancer.
Researchers say their findings can have a major and immediate impact on the clinical administration of cancer therapy by introducing new methods of delivering old drugs.
The Harvard researchers used a mathematical model developed by Mohammad Kohandel, a professor in Waterloo’s Department of Applied Mathematics, and Andrew Dhawan, a former Waterloo math undergrad who is now a medical student. The model predicted the populations of cells within tumors developing resistance to therapy.
“It’s an exciting time to be involved in cancer biology as relationships between biologists and mathematicians are now being recognized as critical to the development of . . . cancer management,” said Goldman.
There is a small subset of cancer stem cells (CSCs), well known to be drug resistant, that have been of interest to researchers as they strive to overcome the challenges associated with cancer therapy failure. The research team found that, after exposure to cytotoxic chemotherapy, populations of non-CSCs were acquiring some attributes of CSCs, reorganizing the proteins within them to overcome the cancer therapy. The researchers observed that drugs targeting a specific protein known as Hck, killed a large fraction of these transitioning cells.
“It is an honor to be a part of this important study," said Kohandel. "Application of mathematical and computational models to cancer biology is an exciting and novel area of research which can determine the most effective timing, sequencing and dosage of chemotherapy.”
The lead authors are now working together with Professor Kohandel to unravel even more complexities of cancer chemotherapy to not only achieve better sequences and combinations of existing drugs, but to develop brand new therapies with the use of nanotechnology.

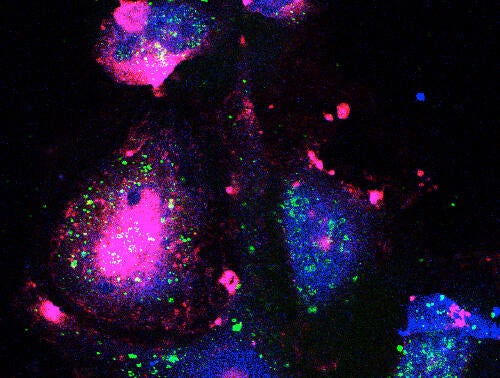 Image depicts drug-tolerant cells. Nuclear translocation of HCK drives anti-apoptotic signaling in response to taxane chemotherapy. This process is initiated by phenotypic plasticity coordinated by cell surface scaffolding involving Caveolin-1 and CD44 glycoprotein.
Image depicts drug-tolerant cells. Nuclear translocation of HCK drives anti-apoptotic signaling in response to taxane chemotherapy. This process is initiated by phenotypic plasticity coordinated by cell surface scaffolding involving Caveolin-1 and CD44 glycoprotein.