
Alumni at busy GTA hospital share COVID-19 challenges
Pauline Bal (Rx2019) didn’t plan to start her new job at Credit Valley Hospital in the middle of COVID-19. But when she showed up for her first day at the hospital, one of the three main Trillium Health Partners sites in the Greater Toronto Area (GTA), it was mid-April and COVID-19 was in full swing.
Pauline was assigned to the COVID-designated medicine and surgical floor, an area created in the hospital specifically for COVID-positive patients so that they wouldn’t come into contact with others in the hospital.
“I quickly learned that COVID doesn’t discriminate,” she says. “Patients with comorbidities that would have typically been treated elsewhere – like renal patients going to the nephrology floor – were instead sent to us if they were COVID-positive.”
The variety in patients meant Pauline had to get up to speed quickly, determining how to manage not just COVID-19, but also the myriad of other conditions patients have. She also collaborates with her health-care colleagues to ensure that medications like antibiotics continue to be used judiciously.
Adding to the challenge of working the COVID-19 floor was the fact that visitor restrictions were in place.
“Patients can’t see their loved ones,” Pauline says. “So, we had to be creative to keep morale up. One morning everyone on our team sang happy birthday to one of our isolated COVID-19 positive patients. It was a small act of kindness, but it sparked smiles!”
COVID-19 changing how patient care happens in the hospital

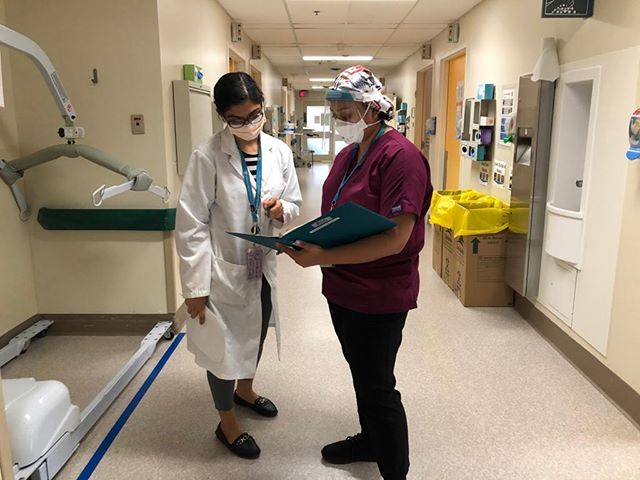
Before COVID, Vincent Vuong (Rx2017, pictured right) was the pharmacist covering a general medicine floor where he saw a variety of patients with conditions like pneumonia, congestive heart failure, kidney injury and more. He was part of an interprofessional team where he went on patient care rounds, resolved medication-related issues and consulted with health-care providers and patients when high-risk medications were used.
But by mid-March, Vincent’s workplace was fundamentally altered. Processes were put in place requiring that rounds were conducted via teleconference or with participants physically-distanced across a room. When meeting with patients, Vincent now phones the patient’s room instead of speaking face-to-face.
“We’ve also developed a process called medication bundling,” he says. “We adjust the dosing times of medications to minimize the frequency of nurses going into patient rooms to administer medications. The goal is to reduce close contact whenever possible.”
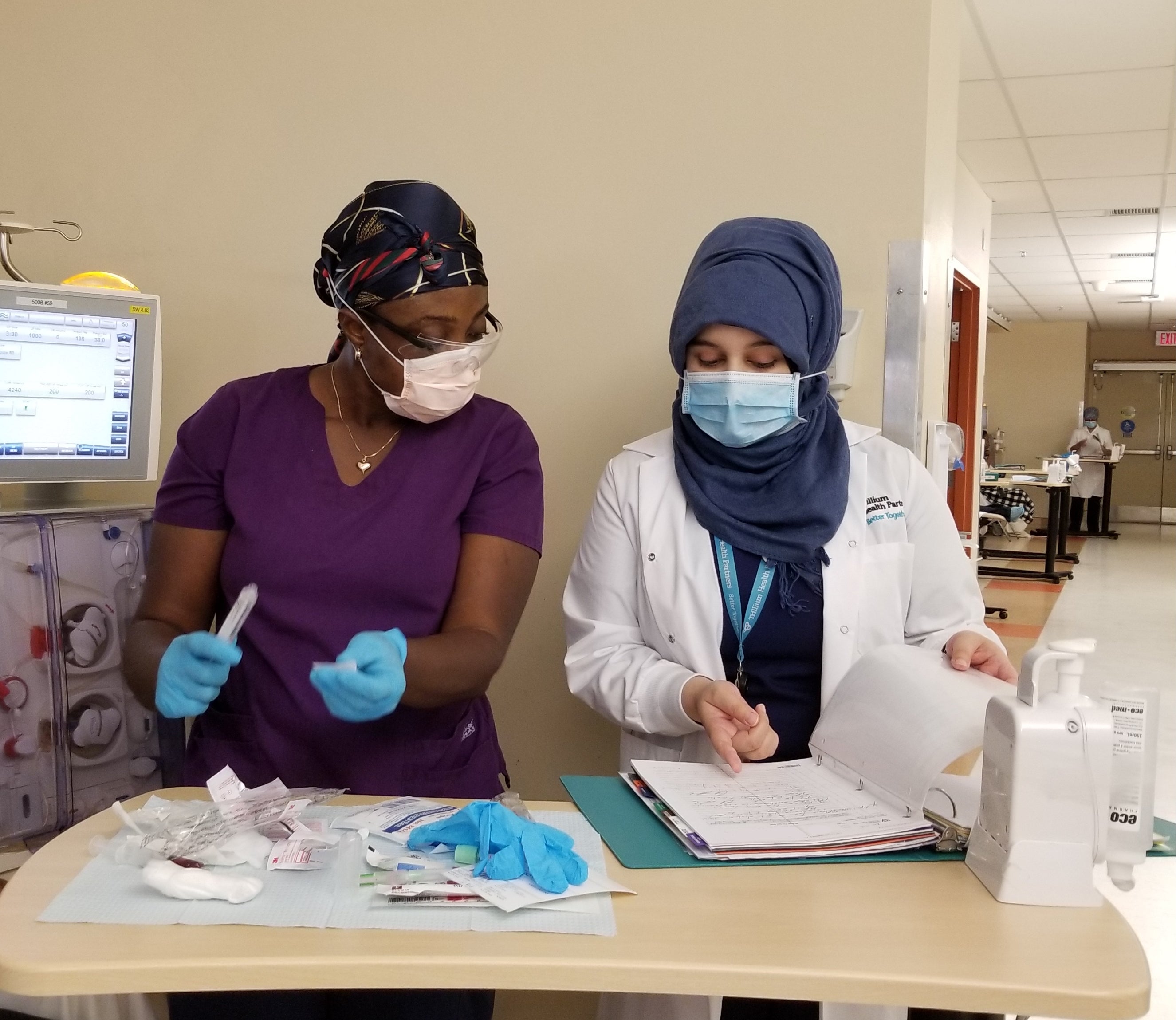
Arpita Desai (Rx2015) and Amna Al-Khayat (Rx2017) have also adapted to the different workflows that COVID necessitates. Amna is a renal pharmacist, and in pre-COVID times she completed in-person medication reviews with patients at clinics, reviewing bloodwork and collaborating with her team to ensure appropriate dosing and medication use. Arpita, who supports the inpatient medicine and nephrology units at Credit Valley, also conducted face-to-face consultations patients, gathering information to make informed medication decisions.
These conversations now happen remotely, through teleconference with patients and health-care teams.
“We understood that our most of our renal patients have multiple health complications that place them at a high risk of contracting the virus and suffering severe complications,” Amna says. “We made a decision to limit our in-person interactions with the patients unless absolutely necessary.”
Where there were once four renal clinic pharmacists on-site at all times, the hospital now only has two, with the other two working remotely.
“Policies and procedures changed quickly,” Arpita (below, left) says. “It’s been challenging to adapt to the new normal — enforcing social distancing at work, virtual meetings, and the new work wardrobe of scrubs and PPE, when necessary.”
Challenges at work and at home
The pandemic has created professional challenges, but it has also added personal ones.
“My parents are elderly, and certainly one of the biggest challenges of all this is the fear of contracting COVID myself and spreading it to loved ones,” Vincent says. “Since COVID outbreaks have occurred in other health-care institutions in Ontario, I’ve avoided visiting my parents for months.”
Being a front-line health-care worker means working with COVID-positive individuals, and the fear of exposure is always present.
"At one point, I was exposed to a COVID-19 case and had to be quarantined for few days while waiting for the test result which ultimately was negative," Amna (below, right) says. "Until I got my result, I couldn't stop worrying that I might have had the virus and spread it to others. Fortunately, I had much support from my colleagues at work and family at home that truly helped me get through the worst of this pandemic.”
The social and professional demands of COVID are exhausting. Vincent was even more disheartened in April when the Ontario government did not include pharmacy staff in the temporary pandemic pay raise announced for front line and support workers. After giving it some thought, Vincent and his coworkers realized that a potential contributor to this decision could be that policy makers and the general public were not aware of the key role pharmacists and pharmacy technicians play.
“We decided to start social media accounts to shine a light on the vital role that pharmacy staff play in keeping our patients and community safe,” he says. “Through Phocus on Pharmacy, we’re sharing images and stories of our contributions, and we welcome and photos and videos from pharmacists and pharmacy technicians across Canada.”
Follow @PhocusOnPharmacy on Instagram, Facebook and Twitter to see Vincent, Pauline, Amna, Arpita and other pharmacy professionals are supporting Canadians throughout COVID-19.
A strong partner of Waterloo Pharmacy
Trillium Health Partners have been a supporter of Waterloo Pharmacy since 2009 when they first began hiring co-op students. Since then they have provided stellar learning experiences for over 80 co-op and 4th year patient care rotation students
“We’re so grateful to have such a strong partnership with Trillium,” says Anthony Miller, Experiential Learning Coordinator for co-op. “They have consistently hired and mentored our students, upwards of an astounding 75 paid work terms since 2009 and ensured that they have rewarding and informative work terms. It’s encouraging to see the experience come full circle with alumni of our program practicing as pharmacists there and supervising their own Waterloo Pharmacy students.”