
PhD candidate blends engineering and biology in award-winning research project

When he was a young boy growing up in Burkina Faso, Yannick Traore’s dad didn’t like to buy him toys. Yannick had a habit of taking things apart just to figure out how to put them back together. Even as a child, he needed to understand how things worked.
Today, Yannick’s putting that curiosity to good use as a PhD candidate in Prof. Emmanuel Ho’s lab.
“I appreciate that in Dr. Ho’s lab I’m not confined to one thing,” he reflects. “My work requires me to approach a problem from both the biology side of things and the engineering side. Combining these ideas is rewarding and exciting – I meet lots of people from different fields and faculties, and I bring a unique perspective to these conversations.”
Yannick was recently awarded a Canadian Graduate Scholarship for his doctoral work through the Natural Sciences and Engineering Research Council of Canada (NSERC), one of Canada’s three major government research funding bodies. This prestigious award allows Yannick to advance his work on developing unique treatments for HIV.
“My family is originally from Burkina Faso, and HIV is a big problem in many parts of the developing world,” he explains. “As a researcher, I’m trying to make a difference and develop tools and treatments that can help people.”
That’s what drew Yannick to working with Prof. Ho as a Master’s student at the University of Manitoba and to follow him to the University of Waterloo in 2017.
“Emmanuel’s lab was the perfect place where I could combine my interests and tackle the problem of HIV. The best thing about working with him is that he gives you the opportunity to explore your ideas.”
On the biology side, Yannick and the Ho lab have developed a solid-lipid nanoparticle gene therapy that will prevent the transmission of HIV. As HIV is a sexually transmitted disease, the team developed a therapy to specifically targets cells in the genital tract where transmission occurs.
First, the researchers load nanoparticles with a customized form of small interfering ribonucleic acid (siRNA) that they designed. The nanoparticles are programmed to target T cells in the female genital tract – these are the cells that HIV typically binds to when transmitting the disease. The nanoparticles bind to the T cells and release the custom siRNA treatment. That treatment knocks down a gene that causes a receptor on the T cells to appear; without that receptor, HIV has nothing to bind to and transmission does not take place.
“We have been developing the various parts of the siRNA treatment and nanoparticle delivery system over the last few years,” Yannick explains. “My current work involves refining the design of the intravaginal ring that contains the medication.”
The intravaginal ring is where Yannick’s engineering expertise comes into play. The team has the nanoparticles that can deliver the siRNA, but how do they get those nanoparticles into the genital tract to begin with? Prof. Ho’s lab has been experimenting with small rings made of medical grade plastic that can be loaded with the nanoparticle siRNA treatment and self-inserted by women prior to sexual intercourse.
The rings are a socially-conscious solution as well. Many who are infected with HIV are sex trade workers or live in places where women may have less say in decisions to use contraception such as condoms. Traditional HIV medications such as PrEP are expensive and hard to access in the developing world. Thus, a self-inserted device that can be used without the knowledge of a sexual partner is a promising solution. The medication would be released through the walls of the intravaginal ring and into the genital tract, preventing HIV transmission.
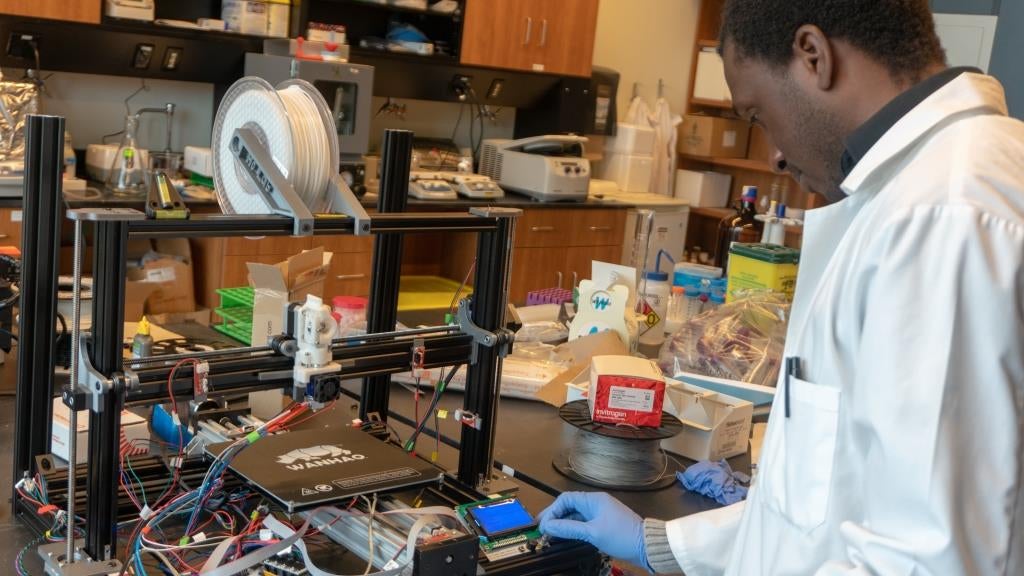
Yannick entering instructions on the lab's home-built 3D printer.
“To maximize the safety and efficiency of intravaginal rings, I’m developing a ring that will be able to detect changes in the pH levels within the vaginal tract,” Yannick explains. “During sexual intercourse, pH increases. If the ring can respond to changes in pH, we can ensure that it is only releasing medication when the medication is actually necessary.”
Designing a ring that only releases medication during sexual intercourse achieves two positive outcomes. Firstly, it prevents continuous release of the siRNA treatment, ensuring that the women’s genital tract does not experience significantly increased toxicity. Secondly, it conserves the amount of medication used, increasing the lifespan of the device and reducing drug costs.

Examples of the different types of intravaginal rings designed by the Ho lab over the years.
The intravaginal rings are created through 3D printing. Yannick is currently testing different kinds of plastic to see which types can respond to pH changes in the environment while also allowing for controlled release of nanoparticles through the plastic membrane.
“Creating designs for 3D printing was a skillset I taught myself in grad school,” says Yannick. “I worked with others in Prof. Ho’s group to develop these skills, and I’m very excited to see where this technology goes in the future.”
The lab group is currently preparing to test their device in mice, but in order to print such tiny intravaginal rings, Yannick realized that they needed finer control than what their current off-the-shelf 3D printers could provide.
“To have the kind of control, the robust features that we want, we realized we’d have to design our own 3D printer.”
Thus, Yannick and the Ho lab are programming and building their own 3D printer. This task involves a combination of buying commercially available parts and designing and printing original parts on their other 3D printers. Their research on this and other related projects has been funded through both an NSERC grant and a Canadian Institutes of Health Research (CIHR) grant acquired by Prof. Ho.
Working in the Ho lab is the perfect blend of Yannick’s passions, and he’s excited both for his current project and about the possibilities the lab’s new 3D printer will present.
“I think that in the future we’re going to see many applications of bioprinting – 3D printed organs and more – and I want to continue as a researcher both in the HIV space and in exploring 3D printing’s applications.”