
Waterloo Pharmacy researcher combines new medical device technology with old medications to combat HIV
36.9 million people worldwide were living with HIV in 2017. In the same year, 1.8 million people became infected and 940,000 people died from AIDS-related illnesses. Despite the existence of antiretroviral therapy to treat HIV, the disease continues to exact a staggering cost on human life, so much so that combatting HIV and AIDS is one of the United Nations Sustainable Development goals for health.
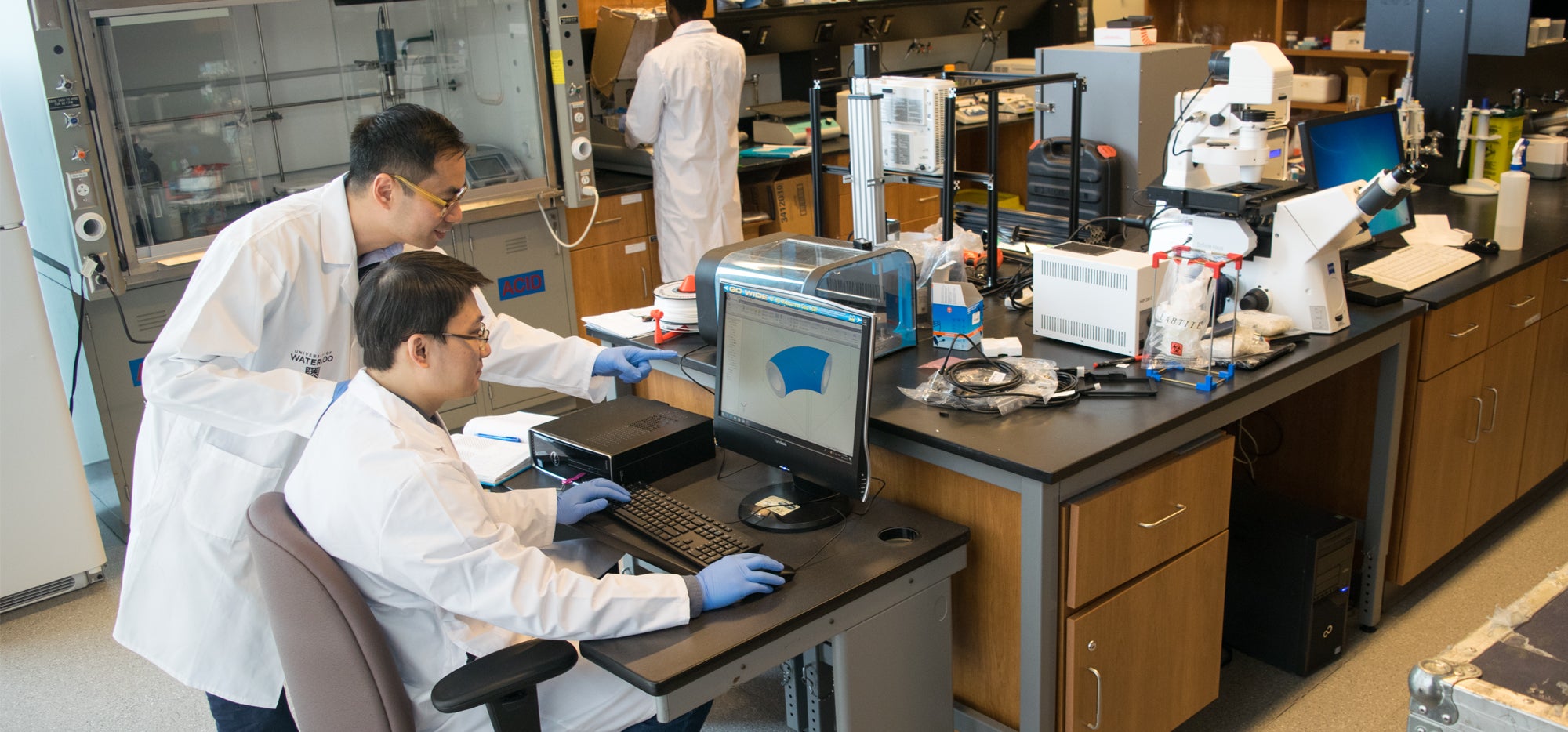
Prof. Emmanuel Ho’s research aims to curb the transmission of HIV by examining new ways to use old medications. His project team recently received two million dollars in funding from the Canadian Institutes of Health Research (CIHR) to build on their existing findings.
“This funding will allow us to examine a combination therapy strategy for preventing the spread of HIV. We’ll be expanding on previous work to test how conventional anti-HIV medications can be used in conjunction with common anti-inflammatory medications to slow the spread of this deadly disease,” says Ho, who is co-principle investigator on the grant along with Prof. Keith Fowke at the University of Manitoba.
In previous studies, Ho and Fowke have made several key findings regarding HIV transmission. First, they determined that even when people were taking antiretroviral HIV medications, they could succumb to infection if they experienced a high amount of inflammation in the genital tract. Inflammation in the genital tract activated a specific kind of cells which HIV likes to target, resulting in increased rates of infection.
For their next steps, the researchers knew they had to find a way to decrease inflammation and thereby decrease the activation of HIV-target cells in the genital tract. They turned to acetylsalicylic acid, or aspirin, and studied how it affected inflammation in healthy women living in Nairobi in Kenya, a country with a high incidence of HIV and AIDs-related death.
“Aspirin is cheap and accessible, with a long history of drug safety. Taking one pill a day was manageable for the women in the study,” explains Ho.
In order to be successful, global health solutions need to be more than just effective – they also need to be affordable and scalable. These were some of the reasons that made aspirin an ideal drug of study. They found that a regimen one aspirin a day decreased inflammation in the women’s genital tracts, resulting in fewer cells for HIV to target. These are the findings their current CIHR-funded research will expand on.
“We know that aspirin has decreased the presence of HIV target cells in some women,” says Ho, “and now we want to expand that to women who are known to have high levels of genital inflammation such as female sex workers. Will taking a daily anti-inflammatory like aspirin decrease the amount of HIV target cells in these women? Will aspirin have this affect while the women are taking anti-HIV drugs as pre-exposure prophylaxis (PrEP)?”
“These women represent a population that is, unfortunately, commonly exposed to HIV,” says Ho. “We wanted to explore a prevention strategy that could be easily adopted by this population, in situations where the women might not have significant sway over decisions about condom usage, and in places where many medications are not easily accessible.”
While examining these immediate effects of a daily aspirin regimen, Ho will also lead additional studies that explore longer term outcomes. His team will use laboratory mice to understand exactly how the aspirin is affecting the HIV target cells in the genital tract. They will also infect the mice with HIV to determine the efficacy of the aspirin regimen in preventing HIV transmission.
The researchers also plan to go one step further in terms of methods.
Taking a drug daily can be challenging for some people, especially for those in unstable living conditions. Therefore, we plan to examine other methods of delivering the daily acetylsalicylic acid treatment.
Ho’s lab has created an intravaginal ring that can be loaded with the medication and discretely inserted by a woman into her genital tract. It would deliver the anti-HIV drug and an anti-inflammatory drug simultaneously.
“Funding from this grant will allow us to understand the role of aspirin in regulating genital inflammation and will provide us with important information towards the development of new HIV preventative strategies,” says Ho.