Professor Jamie Joseph receives CIHR funding to examine root cause of type 2 diabetes

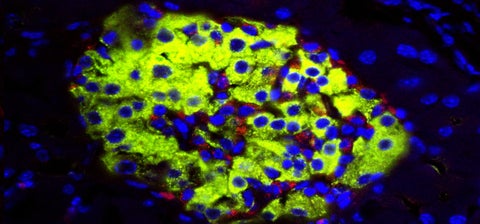
A flourescent image of the islets of Langerhans.
As many as 1 in 4 adults are living with undiagnosed type 2 diabetes mellitus. This chronic condition usually develops in adulthood and can lead to vision damage, organ damage, and even amputation in late stages. Despite its prevalence, the underlying mechanism that causes type 2 diabetes to develop is not completely understood, which makes treatment challenging.

In type 2 diabetes, sugars are not stored properly in the body’s muscle tissues and liver cells. Sugar, or glucose, is absorbed into the body’s bloodstream after a person eats or drinks. The body’s cells need that glucose to function, but glucose cannot enter the cells without the help of a hormone called insulin. Insulin unlocks the cells, enabling glucose to enter and be stored for later use.
The beta cells that Joseph studies are essential in this process. Beta cells are found in a specific part of the pancreas called the islets of Langerhans.
“Insulin is released by the pancreas, but in order for the pancreas to know when to release insulin, it has to detect how much glucose is currently in your bloodstream,” explains Joseph. “Beta cells facilitate this process – when they’re working properly, these cells detect glucose in the bloodstream and tell the pancreas to release insulin.”
In people with type 2 diabetes, beta cells often stop working properly. The pancreas doesn’t accurately detect how much glucose is in the bloodstream, and insulin is not released in sufficient quantities to do its job. Glucose builds up in the bloodstream but the parts of the body that need sugar for energy – such as the muscles – don’t receive enough of it because there is insufficient insulin to unlock cells and let the glucose enter. As a result, people with type 2 diabetes tend to feel tired and suffer other symptoms like increased urination and blurred vision.
“We’re examining why and how these beta cells become defective,” says Joseph. “This current CIHR grant will help us study a protein called prolyl hydroxylase domain (PHD). We believe this protein helps beta cells detect glucose and tell the pancreas to secrete insulin.”

Monica Hoang, a PhD candidate in Joseph's lab, studies the islets of Langerhans through a microscope.
To study PHD, the Joseph lab uses transgenic mice – mice that have had their genome altered through genetic engineering. The researchers mark the gene that creates PHD in the animals’ genome and are able to delete the gene entirely by injecting the mice with a medication at a pre-determined time. This process helps the team simulate the adult onset of type 2 diabetes, as the PHD gene is typically deleted at about 8 weeks into the experiment.
After deleting the gene, the scientists examine what happens to the beta cells and whether or not diabetes begins to develop. In Joseph’s recent studies, PHD proteins have been shown decrease prior to the development of diabetes.
The next step is to examine how well a mice model compares to a human one. To do this work, the lab group uses human cells from the islets of Langerhans and conducts similar experimentation.
This work is fundamental to our understanding of how beta cell dysfunction occurs. It’s useful because it can then go on to inform drug therapy. If we know that PHD, or the absence of it, impacts beta cell function, and subsequently type 2 diabetes, we give drug developers a new target for type 2 diabetes medication.
Ideally, such medications could prevent the loss of PHD and thus help ensure beta cells continue to work properly. Though beta cell dysfunction may be just one of the many complex potential causes for diabetes, Joseph believes his lab’s findings will inform both future research and eventual treatment for type 2 diabetes.