The world of health care is rapidly changing as big data, artificial intelligence (AI), new technologies and systems disrupt traditional health care. The future of medicine is being reimagined with these advancements. In the Faculty of Mathematics, researchers, students, and alumni are developing new ways to look at the world of medicine and health care. This is impacting predictions, precision, and prevention and treatment and can help people live healthier lives.
Predicting outbreaks and outcomes

In the Department of Applied Mathematics, Professor Chris Bauch uses mathematical models that include social behaviours to predict the emergence and evolution of infectious diseases within host populations. “By thinking about treating disease systems as it connects to social systems, we have a better appreciation of how social reactions to social diseases can influence which strains become prominent in the population,” said Bauch. With this approach, researchers can better anticipate how a virulent pathogen strain may emerge based on how humans attempt to control the spread of the disease.
Researchers in the same department are also looking at how cancer cells evolve. Associate Professor Mohammad Kohandel and Professor Siv Sivaloganathan use a mathematical analysis called evolutionary dynamics to look at how malignant mutations evolve in both stem and non-stem cells in colorectal and intestinal cancers. Using mathematics, they map out the evolution of cancer to provide oncologists with a road map to track the progression of a particular cancer. This work could lead to tailored treatments that target the cells effectively and help avoid the drug-induced resistance known to develop in many cancers.
Numbers aren’t the only indicator that can be used. A study co-written by Joel Dubin, an associate professor in the Department of Statistics and Actuarial Science, found that sentiments in nursing notes are good indicators of survival in ICU patients. Dubin and his collaborators used an open-source sentiment analysis algorithm to establish if statements were positive, neutral or negative. They then used a multiple logical regression model to fit the data to show a relationship between the measured sentiment and 30-day mortality rate.
At a time when health care systems are under pressure to plan more effectively for the future, early treatment is key to ensuring less strain on the whole system. Mathematical predictions can help avoid outbreaks and improve outcomes for patients.
Precision improves outcomes
The field of precision medicine continues to grow. Professor Bin Ma is developing software to discover and measure disease biomarkers from the Data Independent Acquisition (DIA). The DIA method measures protein biomarkers in patient samples using mass spectrometry. Health care practitioners need software to analyze the vast quantities of data produced by this method. Ma’s bioinformatics software will reduce health care costs, allow earlier disease detection, and facilitate optimized selections of treatments for each patient.
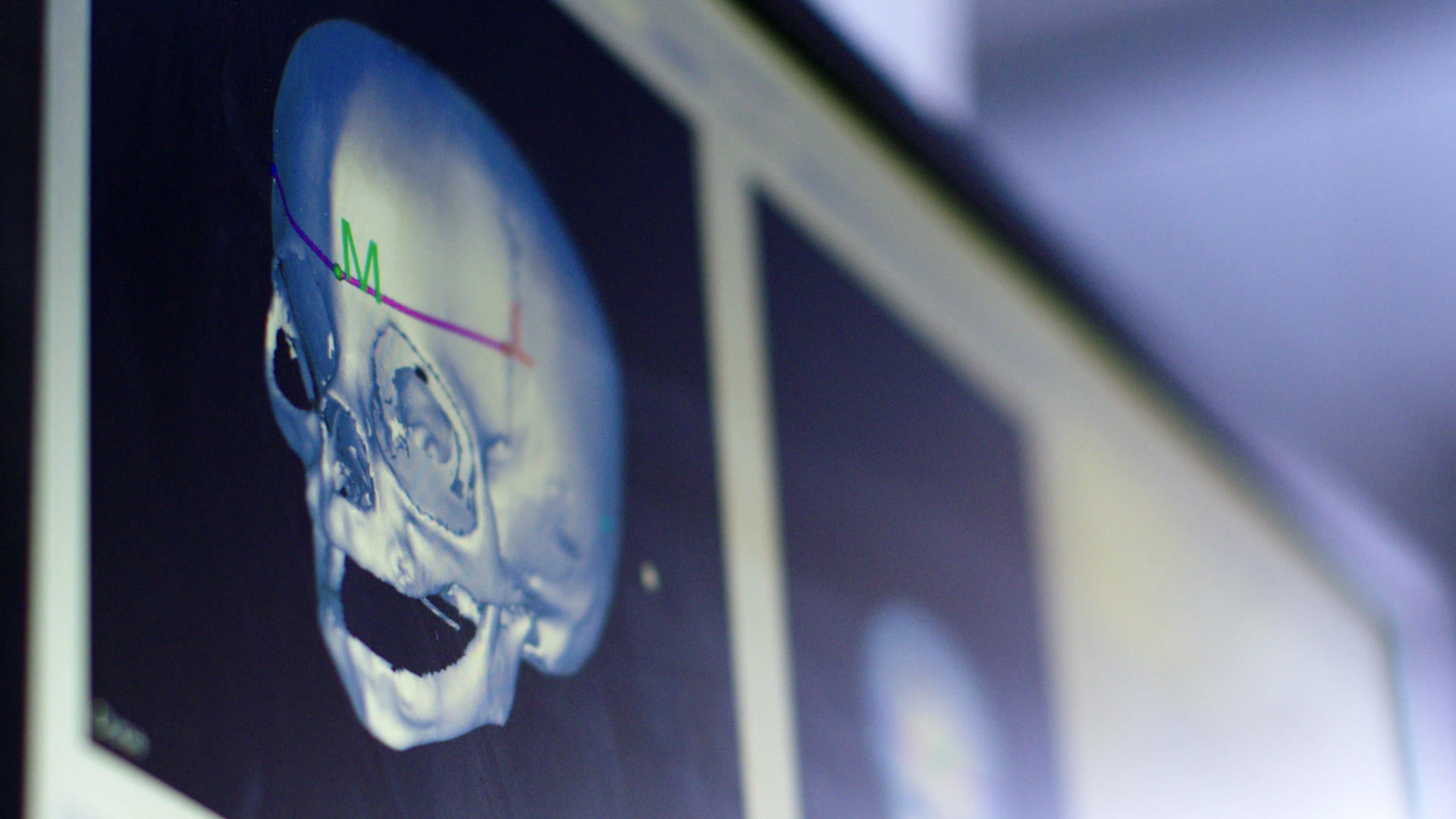
Precision is of the utmost importance for high-risk surgeries. Two professors in the Department of Combinatorics and Optimization are working with Sick Kids hospital to equip surgeons with precise algorithms to plan and carry out surgeries on infants with craniosynostosis. Affecting one in 25 infants, craniosynostosis causes some or all of the bones in a child’s skull to fuse prematurely which can impact brain growth. Professor Jochen Koenemann and Associate Professor Ricardo Fukasawa developed an algorithm for efficient and accurate plans for the cut locations on an infant’s skull and the reconfiguration of the pieces of the skull for a more typical shape. “This project has provided a rare opportunity for us as mathematicians to contribute in a meaningful way and improve the lives of young children,” noted Koenemann.
When precision is needed for medical applications, mathematical models can help. Cameron Meaney, a PhD candidate in the Department of Applied Mathematics has led the development of a new mathematical model that will significantly increase the number of tumour cells killed during radiation treatment. The model uses information about where the majority of the cells in a tumour are located allowing for radiation treatment to be administered to the densest area. The model showed that administering the total allowed radiation, when administered over a small area at high strength where the cells are most dense, kills more cells as opposed to spreading it over a big area with semi-weak strength.
When individualizing medicine or finding optimal ways to improve a treatment, precision matters. Doctors depend on the precision of mathematics and the innovations of a computer science to improve health care outcomes.
Preventing outbreaks and developing innovative treatments

Kevin Church, a PhD candidate in the Department of Applied Mathematics, discovered a more effective way to prevent disease outbreaks. If the majority of the population in a particular region are vaccinated at the same time, practitioners have a better chance of controlling the outbreak. Church and his supervisor Professor Xinzhi Liu, modified a mathematical model building around the idea of pulse vaccination, a disease control policy where, at certain times, a portion of the population is vaccinated altogether. It could help manage flu and measles outbreaks. The timing of vaccinations is critical in the control of infectious diseases.
Translational models can also be used as a way to inform strategies for the clinical human setting. An alumnus from the same department, Colin Phipps, is now a senior researcher at Abbvie and works with clinical data to build translational models. His role is to develop and simulate models, run the analyses, and present results to clinicians. “As the field expands with a myriad of new and more complex treatment options for patients, we see a need for quantitative analysis and more mathematicians and computer scientists tacking relevant problems in medicine,” said Phipps.
Using a computational model is another way to improve health care. Anita Layton, Canada 150 Research Chair in Mathematical Biology and Medicine in the department of applied mathematics, has developed the first computational model of the human kidney. With this method, clinicians can test treatments for drugs that target kidneys, such as diabetes medications, before it goes to a clinical setting. Using a computational model is less expensive to run, presents less risk to patients, while better analyzing long-term effects of the drugs.
Mathematical models can also be combined with AI to develop tools for treatment. Jesse Hoey, a professor in the David R. Cheriton School of Computer Science leads a team using mathematical models of human interaction with AI to aid older adults living with Alzheimer’s disease and dementia. Their virtual assistant automatically monitors a person doing a task and offers verbal prompts to encourage them to start and complete tasks.
If we can find new ways to use math to prevent diseases or develop more effective treatments while reducing risk to patients during clinical trials, it will greatly impact the health care industry and patient wellbeing.
Using mathematics as a microscope and computer models to analyze data and run simulations, mathematicians and computer scientists are crossing interdisciplinary boundaries. Their skills allow them to sift through the data, provide analysis, solve problems and build algorithms, models, and technology. As the volume of data increases and the health care industry continues to look for innovative, cost-efficient solutions,the need for mathematicians and computer scientists with a focus on applied mathematics, data science, bioinformatics, and biostatistics will continue to grow.